
![]() Contributed by Alicia Liang, MD and Rene Duquesnoy, PhD
Contributed by Alicia Liang, MD and Rene Duquesnoy, PhD
![]() Published on line in May 2006
Published on line in May 2006
PATIENT HISTORY:
This is the unfortunate story of a 45-year-old female who been in good health up until 2000, at which point she donated a kidney for her daughter. She was doing well until 2004, when she developed abdominal pain and was found to have a ruptured splenic artery, which necessitated splenectomy. Several days later she developed ischemia of the large bowel and required a subtotal colectomy. After this she suffered from ischemia of the gallbladder and small bowel, and require removal of these organs as well. As the patient is from out of state, she was transferred to a hospital back home, where further evaluation for the ischemia showed positive tests for heparin-induced thrombocytopenia. She required several additional procedures for fistulae formation and adhesions, and soon after also developed short-gut syndrome and liver failure. She was then referred in October 2004 for evaluation for transplantation.
Initial evaluation for a transplant consists primarily of determining the patient's human leukocyte antigen (HLA) profile, and determining if the patient has preformed antibodies for any specific antigens. Patients who are nulliparous often have fewer antibodies, as are patients with fewer blood transfusions. The patient's HLA type is as follows:
On 12/2004, the patient has the following preformed antibodies:
The donor's HLA type is as follows:
A donor was identified, and the patient had a crossmatch performed that was negative for both B and T cells. (This test will be further discussed later.) The patient was transplanted with a liver, pancreas, stomach and small bowel from a cadaveric donor early in 2005.
However, in early 2006, she began to experience chronic renal insufficiency and acute renal failure, thought, in part, to be secondary to FK 506 toxicity; an evaluation for a renal transplant was begun. The patient's sibling was identified as a potential donor and an evaluation for HLA compatibility ensued. His HLA type is as follows:
The patient had an antibody analysis performed before her first transplant; however, as the first donor had multiple HLA mismatches, there is a possibility that the patient has formed new antibodies against foreign antigens. Therefore, a second antibody analysis using both enzyme-linked immunosorbent assay (ELISA) and quick panel-reactive antibodies (QPRA) was performed. The recipient's updated antibody profile is as follows:
This antibody panel is dramatically different from the initial antibody panel. Are the prior antibodies of clinical significance? [Answer]
The two methods of testing commonly used include the lymphocytotoxic crossmatch and flow cytometry. These tests are utilized only after a specific donor is identified - these are not a part of the screening evaluation:
The first of two tests performed is the lymphocytotoxic crossmatch. This involves combing recipient serum with potential donor lymphocytes. The donor's blood is obtained, and is purified so that only T and B-lymphocytes are in the sample. The samples are also evaluated in the presence of DTT, which essentially breaks up the pentameric IgM, which is an antibody of minor significance. The serum and lymphocytes are incubated together, and the results are read as positive or negative. The results are as follows (Figure 1):
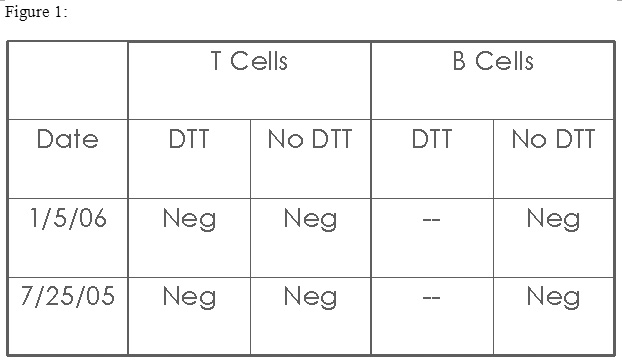
As the results of the crossmatch are negative, can the patient be transplanted using her brother's kidney? [Answer]
Therefore, a second test that evaluated cross-reactivity between the patient and her sibling was performed: flow cytometry. The premise of the test is the same, and therefore the set-up is very similar. Basically, whole blood from the potential donor is purified of the T and B cells, and these cells are incubated with the patient's serum. This test is specific for IgG antibodies, therefore and incubation with DTT is not necessary. However, the results are reported as Mean Channel Shift, and values above a preset number are positive, and below that number the result is negative. The patient's results are as follows (figure 2):

Does the positive flow crossmatch still suggest the patient may not be transplanted?
There is a possibility that the antibodies are clinically irrelevant autoantibodies. For example, the patient may have cytotoxic IgG or IgM autoantibodies that may cause the cytotoxic crossmatch test to be positive, but would not actually be a contraindication to transplantation. However, because this was not the case (the cytotoxic crossmatch was negative, but the second, more sensitive test, was positive), then the test result is real. Therefore, as these tests obviously have some variability, it is very important that the laboratory performing these tests has ways in which to confirm the results.
Furthermore, to confirm the validity of the test result, a correlation can be made with the clinical scenario: the patient has an antibody to DR53, and her brother has a DR53 antigen, therefore, the flow cytometric result is logical.
Because of these results, the patient did not receive her brother's kidney.
Bibliography:
Gebel HM, Bray RA, Nickerson P. 'Pre-Transplant Assessment of Donor Reactive, HLA-Specific Antibodies in Renal Transplantation: Contraindication vs. Risk.' American Journal of Transplantation 2003; 3: 1488-1500.