![]() Contributed by Jennifer M. Jones, MD and Lirong Qu, MD
Contributed by Jennifer M. Jones, MD and Lirong Qu, MD
CLINICAL HISTORY
A pediatric patient with no significant past medical history presented with one week of persistent fevers, cough, abdominal pain, and postprandial emesis. On admission, the patient was fatigued, tachypneic, and coughing frequently. Her vital signs were as follows: temperature 38.5°C, pulse 180 bpm, respiratory rate 60 breaths per minute, O2 saturation 88% on room air (required 16 L by nasal cannula to maintain oxygen saturation > 92%). Chest X-ray on admission was notable for consolidation throughout the right lung with displacement of the right mainstem bronchus.
Her complete blood count on admission was significant for mild anemia (11.2 g/dL) and white count within normal limits (5200 cells/μl). Her hemoglobin and platelet count declined through her early admission as follows:
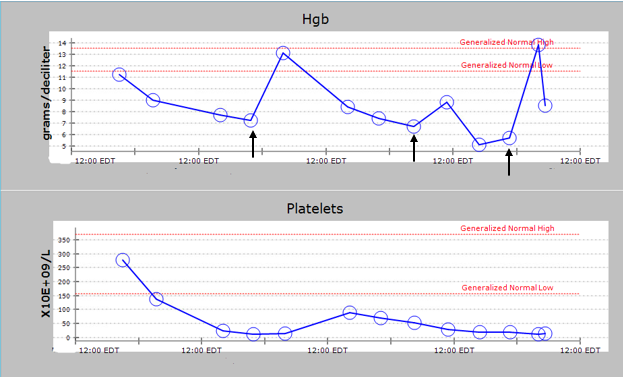
She required three red cell transfusions (black arrows). Peripheral smear demonstrated poikilocytosis, red cell fragments, and schistocytes. Hemolysis work up was significant for undetectable haptoglobin, indirect hyperbilirubinemia, and elevated LDH (2500 IU/L). Given concern for microangiopathic hemolytic anemia, ADAMTS13 activity was ordered and resulted at 44%. The patient subsequently developed acute renal failure (Cr 3.2 mg/dL). This constellation of clinical symptoms and laboratory findings was concerning for pneumococcal-associated hemolytic uremic syndrome.
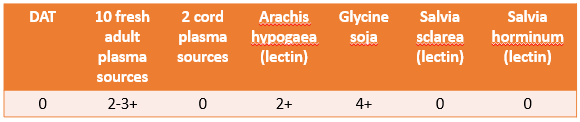
The blood bank requested a sample for additional testing given her presumed diagnosis. Results of these are as follows: