
![]() Contributed by Jacob Jerome, MD and William Pasculle, ScD
Contributed by Jacob Jerome, MD and William Pasculle, ScD
CLINICAL HISTORY
A woman in her 50s presented to her primary care physician with several days of right ear pain. She was afebrile with stable vital signs, and denied any headache, neck pain, or nuchal rigidity. Otoscopic exam revealed erythema and bulging of the tympanic membrane. She was diagnosed with acute otitis media and prescribed azithromycin.
One day later, the patient presented to the emergency department with severe headache and neck pain, somnolence, and expressive aphasia. She was febrile and demonstrated nuchal rigidity on physical exam. Labs were notable for leukocytosis (17.6) with left shift. Chest x-ray showed no evidence of acute processes and urinalysis was unremarkable. Stroke workup was also pursued and was unremarkable. Given concern for meningitis, lumbar puncture was performed and showed turbid CSF with elevated protein (401), glucose (65), elevated WBCs (2950; 97% PMNs). Gram stain of the CSF showed moderate WBCs, but no organisms. Empiric treatment for meningitis was then initiated, including vancomycin, ceftriaxone, and acyclovir.
Bacterial culture of the CSF isolated pale grey, mucoid, smooth, and semi-transparent colonies that grew on chocolate agar (Figure 1), but not blood agar.
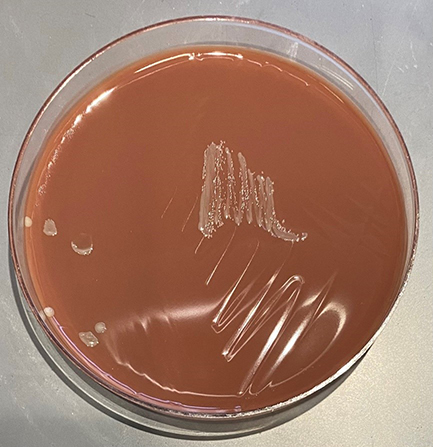
Figure 1. Growth on chocolate agar.
Gram staining of the isolate revealed small, pleomorphic Gram-negative rods (Figure 2).
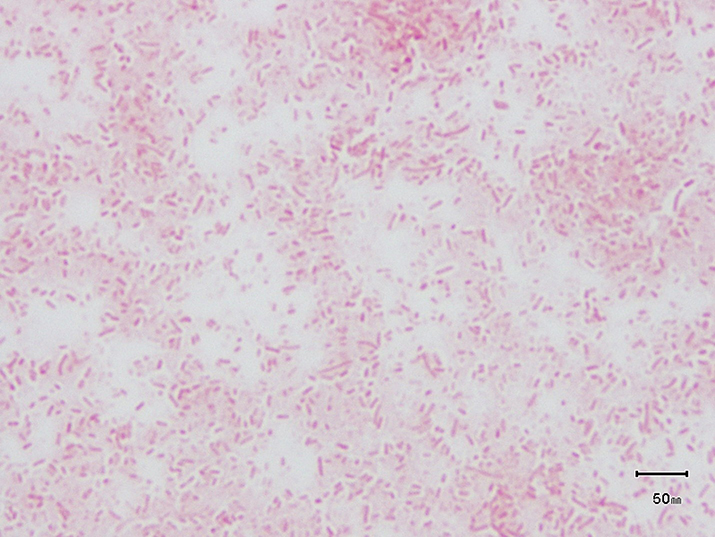
Figure 2. Small Gram-negative rods
MALDI-TOF was then utilized for definitive organism identification. Given these findings and the identification of this organism, vancomycin and acyclovir were discontinued, with a plan to continue ceftriaxone for 10-14 days. The patient experienced symptom improvement shortly after initiation of antibiotics and had no residual symptoms after finishing the course of ceftriaxone.